

Referral for radiofrequency catheter ablationĬatheter ablation of the slow pathway is recommended in patients with AVNRT (class I recommendation, level B-NR evidence)Ĭatheter ablation is recommended in patients with symptomatic focal atrial tachycardia as an alternative to pharmacologic treatment (class I recommendation, level B-NR evidence)Ĭatheter ablation of the accessory pathway is recommended in patients with AVRT or pre-excited atrial fibrillation (class I recommendation, level B-NR evidence)Īn electrophysiologic study is reasonable in asymptomatic patients with pre-excitation to stratify risk for arrhythmic events (class IIa recommendation, level B-NR evidence)Ĭatheter ablation of the cavotricuspid isthmus is useful in patients with atrial flutter that is either symptomatic or refractory to pharmacologic rate control (class I recommendation, level B-R evidence)
#ATRIAL FLUTTER VS SINUS TACHYCARDIA HOW TO#
Patients with SVT should be educated on how to perform vagal manoeuvres for ongoing management of SVT (class I recommendation, level C-LD evidence) Oral β-blocker, diltiazem or verapamil treatment is useful for ongoing management in patients with symptomatic SVT who do not have ventricular pre-excitation during sinus rhythm (class I recommendation, level B-R evidence)Įlectrophysiologic study with the option of radiofrequency catheter ablation is useful for the diagnosis and potential treatment of SVT (class I recommendation, level B-NR evidence) Intravenous use of β-blockers is reasonable for acute treatment in patients with hemodynamically stable SVT (class IIa recommendation, level C-LD evidence) Intravenous administration of diltiazem or verapamil can be effective for acute treatment in patients with hemodynamically stable SVT (class IIa recommendation, level B-R evidence) Synchronized cardioversion is recommended for acute treatment in patients with hemodynamically stable SVT when pharmacologic treatment is ineffective or contraindicated (class I recommendation, level B-NR evidence) Intravenous administration of adenosine is recommended for acute treatment in patients with regular SVT (class I recommendation, level B-R evidence)
Vagal manoeuvres are recommended for acute treatment in patients with regular SVT (class I recommendation, level B-R evidence)

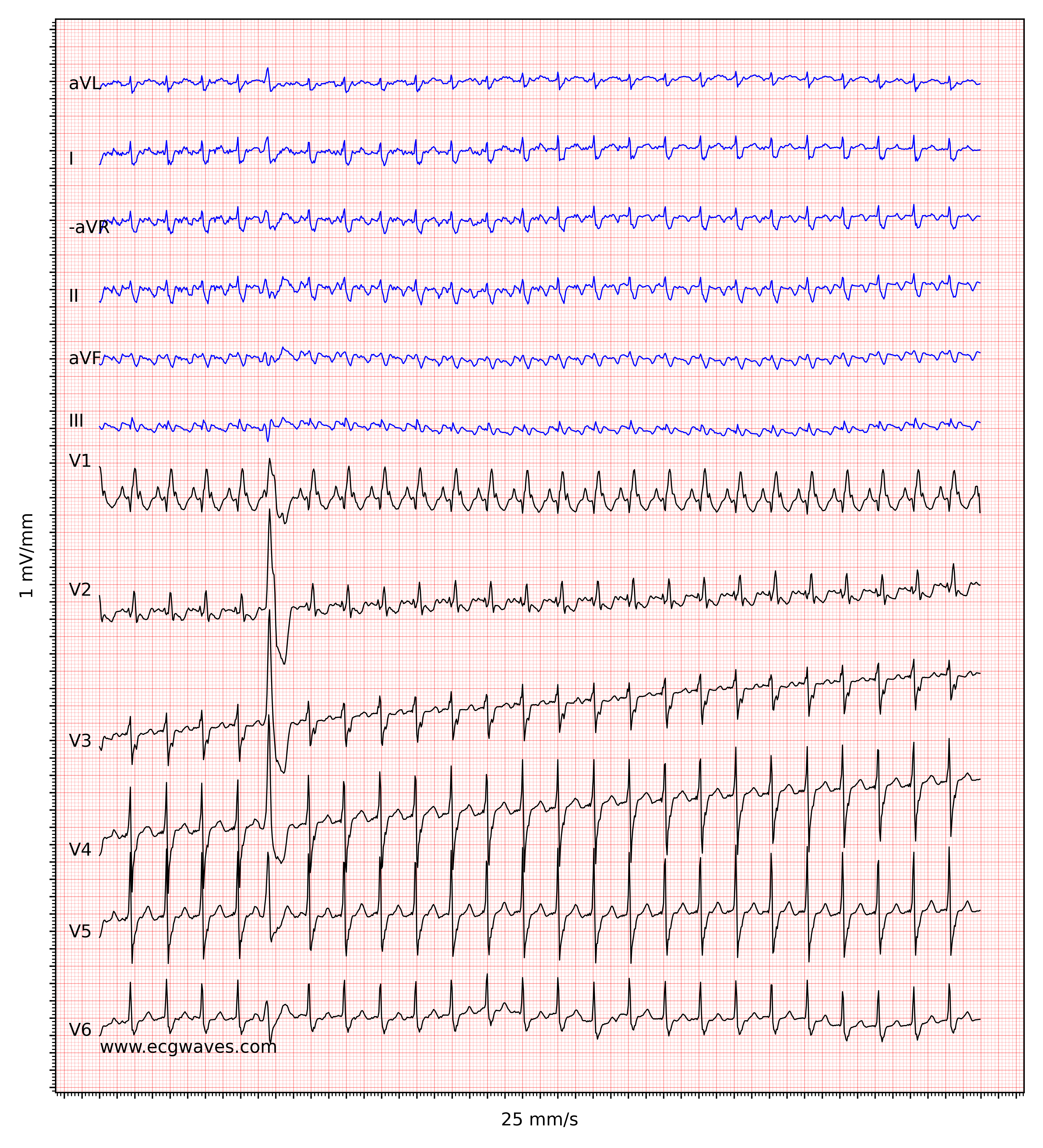
5īox 2: Summary of recommendations from the 2015 guideline of the American College of Cardiology, the American Heart Association and the Heart Rhythm Society on the management of adults with supraventricular tachycardia (SVT) *, 5 Rapid recognition of the underlying rhythm is essential to correct management in the acute setting, including identifying patients who may benefit from definitive treatment with catheter ablation. Occasionally, they may show a wide QRS complex in the case of a pre-existing conduction delay, an aberrancy due to rate-related conduction delay or a bundle branch block. Supraventricular tachycardias are usually narrow-complex tachycardias with a QRS interval of 100 ms or less on an electrocardiogram (ECG). 4 The term paroxysmal SVT denotes a subset of SVTs that present as a clinical syndrome of rapid regular tachycardia with an abrupt onset and termination.

Supraventricular tachycardias represent a range of tachyarrhythmias ( Figure 1) originating from a circuit or focus involving the atria or the atrioventricular node. population and the incidence 35 per 100 000 person-years. 2 In the US, the prevalence of paroxysmal SVT in the general population is 2. 1 Atrial flutter has an overall incidence of 88 per 100 000 person-years, with an increasing incidence in older people, men and people with heart failure or chronic obstructive pulmonary disease. Although Canadian epidemiologic data are lacking, evidence from the United States suggests that they account for about 50 000 emergency department visits annually. Supraventricular tachycardias (SVTs) are common.


 0 kommentar(er)
0 kommentar(er)
